Interdisciplinary work and discussion can yield remarkable results. Fluidda has combined aerospace engineering and biomedical expertise to create a truly unique profile. The company’s Functional Respiratory Imaging (FRI) technology provides, for the first time ever, regional insights into the lungs of patients with any lung disorder. With applications in both clinical practice and drug development, FRI is set to become a new standard tool in pulmonology.
The concept behind Fluidda originated from an extraordinary combination of expertise. CEO Jan De Backer was trained as an aerospace engineer and later found his way into the biomedical field through his father, a pulmonologist at the University Hospital of Antwerp.
“During my studies in aerospace engineering, I specialized in aerodynamics, the science studying airflow around airplane wings and motors,” explains De Backer. “We used computers to simulate how air behaves in the context of aviation. Later on, my father wondered if this technique, the so-called computational fluid dynamics, could be used to model the airflow in the lungs and airways. I decided to do a PhD on the subject and subsequently founded Fluidda.”
Mismatches between therapy and disease occur frequently. FRI now enables us to look inside the lung, identify the problem and its location efficiently and pair it with a suitable treatment.
The ins and outs of FRI
Now, more than 10 years later, Fluidda’s Functional Respiratory Imaging (FRI) technology is well on its way to revolutionize the respiratory field. We asked De Backer for details about this innovative technology.
“FRI is a combination of imaging technologies, such as CT or MRI scans, and computational fluid dynamics. This allows us to simulate the airflow within a patient’s lung and to obtain regional information of the lungs. This is unprecedented, as current lung function tests are breathing tests, which describe the lung as a whole and which leave a lot of information untouched. Based on these breathing tests, doctors prescribe a certain therapy and hope that there is a match with the disease. Unfortunately, mismatches between therapy and disease occur frequently. FRI now enables us to look inside the lung, identify the problem and its location efficiently and pair it with a suitable treatment.
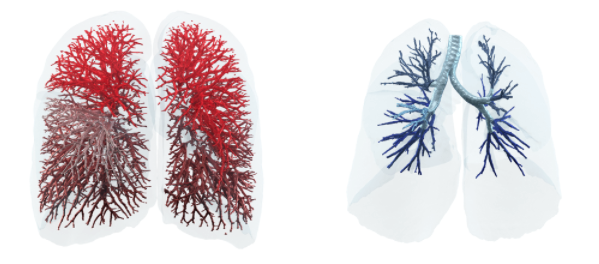
The beautiful thing about the technology is that these CT scanners or MRI scanners are already present in the hospitals. Now we only get a subjective analysis from the radiologist interpreting the CT images, but with FRI we can quantify parameters and retrieve a lot more information from them.”
Although FRI might seem like a niche technology, its applications within the respiratory field are numerous. Not only is FRI relevant for nearly all pulmonary indications (think asthma, COPD, cystic fibrosis, pulmonary hypertension, etc.), it is also extremely valuable in both clinical practice and drug development. De Backer elaborates:
“It comes down to finding the right doctors, those who are motivated to do something new, who are willing to look beyond the status quo.
“In clinical studies, we analyze the CT scans of a group of patients before and after treatment to evaluate the therapy’s effect. The questions that need answering in such a context are: Is this therapy efficient and safe? Should we continue development of our drug? In clinical practice, FRI is used to diagnose individual patients and select a suitable treatment. While we look at the general effect of a treatment on a certain patient group in clinical trials, we go for a personalized medicine approach in the clinical practice.”
Make way for the future!
Unfortunately, bringing innovative technology to the healthcare sector is notoriously difficult, but Fluidda is more than up for the challenge. After many years of pilot studies and test cases, FRI is ready to take the market by storm.
“It comes down to finding the right doctors, those who are motivated to do something new, who are willing to look beyond the status quo. People often use the old technology because they know how it works; they know it’s far from perfect, but they know what to expect from it. If you’re then trying to launch something new, you need a lot of hard proof, data, publications, etc. to convince doctors of your technology. The recent FDA recommendation letter for the use of FRI in lung fibrosis, for example, is an immense support in that quest. Additionally, we launched Broncholab just this week at the ERS International Congress. Broncholab is a web platform where anyone can log in and review some cases where FRI brought significant added value to the table. With Broncholab, everyone can discover the unique FRI advantages.
That was also the reason why we started implementing FRI in clinical trials: It’s much easier to bring innovations into a strictly controlled environment. Now that we have the data and information that shows FRI’s added value, we’re ready to win over the pulmonologists from the clinical practice.”
Setting the bar high
Now that Fluidda has earned its position in drug development and is armed with intellectual ammunition in the form of FRI, the time has come for upscaling. De Backer has ambitious goals for Fluidda’s future:
“We need to make sure that our technology gets implemented more and more in the clinical practice, especially for patients with limited options. FRI needs to become the new standard, a tool embedded in the SOPs. This way, we can build up a database of patients and cases, revealing completely new insights in respiratory disorders. If you succeed in just that, you can revolutionize the field, redefine respiratory diseases by using better, more sensitive endpoints based on FRI. This allows not only for better diagnosis, but also drastically improved drug development and treatment.
In the future, every phase 2 trial in the respiratory domain should make use of imaging tools — preferably together with our FRI technology, of course, but imaging in general has to become standard practice.”


