One in eleven adults around the world has diabetes, according to figures published by the International Diabetes Federation (IDF) in 2017. A research team, led by Professor Decio L. Eizirik (ULB Center for Diabetes Research), has been studying the pathogenesis of diabetes for many years. Working with colleagues from the VUB, the group is on track to have one of its research projects evolve into the spin-off “BetaBild”. The project dates back to 2006, supported by the first call for projects launched by the competitive cluster BioWin.
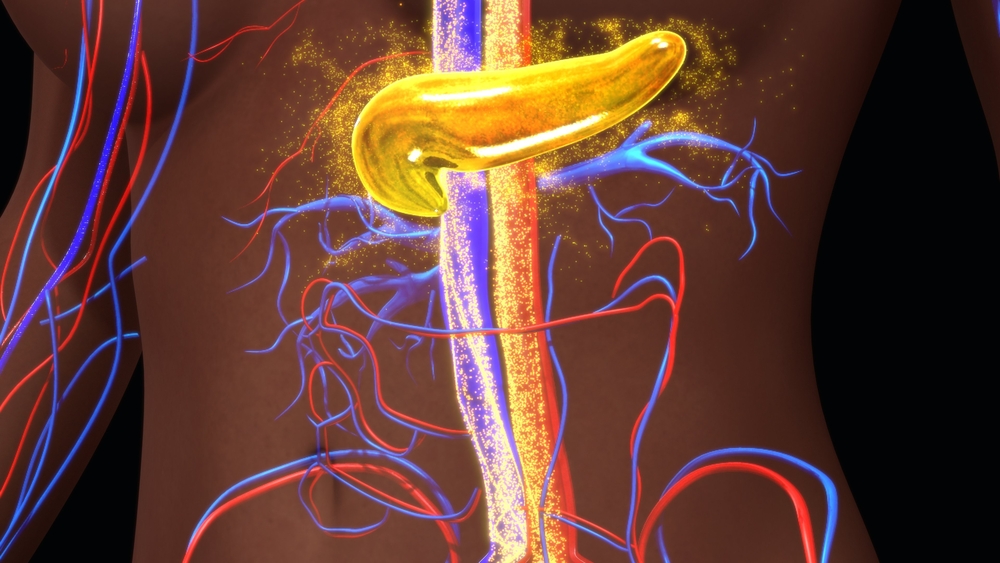
The story began over a decade ago with the launch of Keymarker, the first multidisciplinary research project supported by BioWin. The goal of the Keymarker project was to use functional genomics in order to discover biomarkers for diverse cells, including β cells, for imaging in Type 1 diabetes, cancer, and autoimmune diseases. After the mid-term assessment, a decision was made to focus on quantifying pancreatic β cell mass using imaging.
There is therefore an urgent need for techniques that allow us to quantify β cells non-invasively and directly.
After 12 years, what is happening on β cell research in diabetes?
Professor Decio L. Eizirik, director at ULB responds: “We know that the malfunction and death of β cells plays a vital role in the pathogenesis of different forms of diabetes, but the changes of the cells quantities over time has not yet been accurately determined. The functionality of β cells is measured indirectly, by assessing the C-peptide (a protein co-secreted with insulin) concentration in the blood. There is currently no reliable way to quantify the β cell mass in vivo. The lack of β cell imaging techniques makes it very difficult to assess the impact of new drugs designed to prevent the progressive loss of these cells in diabetic patients. There is therefore an urgent need for techniques that allow us to quantify β cells non-invasively and directly.”
Why is this so difficult to measure?
Eizirik: “One of the obstacles is the relatively small number of β cells: they only account for about 1-3% of the total pancreas mass. These cells are grouped in islets: small micro-organs containing around 50% β cells, as well as several other endocrine and non-endocrine cells. Current medical imaging techniques do not have sufficient resolution to allow imaging of individual islets. To determine the total β cell mass, the only alternative is to employ “chemical imaging”, used to image dopaminergic neurons in patients affected by Parkinson disease.
The quantification of the total mass of β cells would help improve the prevention of diabetes and aid development of personalised treatments for the disease.”
What is your approach?
Eizirik: “There are currently 4 radio-tracers that have been tested in human clinical studies. Unfortunately, they lack precision: they bind to other cell types in the pancreas and are not sensitive enough to quantify the β cell population. We must therefore identify new biomarkers and improve the structure of existing radiotracers.
At ULB, an innovative approach based on identifying isoforms specifically expressed in the β cells is being used to identify new biomarkers. This approach uses transcriptomic data generated by RNA sequencing and compares the results with those obtained from other abdominal tissues that could potentially interfere with β cell imaging, such as the stomach, liver or intestines. So far we have identified three new specific biomarkers for β and α cells: an isoform of the protein FXYD2γ (FXYD2γa), DPP6 (Dipeptidyl Peptidase 6) and a third biomarker currently being validated.
Using this novel approach, we hope to be able to detect and quantify the mass of β cells in vivo in the near future. Combined with other pancreatic biomarkers, like measurement of C-peptide, these imaging techniques will allow better stratification of patients for clinical trials. This will in turn improve prediction and follow up of diabetes evolution in individual patients, ultimately optimizing personal therapeutic strategies for people affected by the disease.”
Why did you decide to create a spin-off?
Eizirik: “We are at a crucial moment: we need to move forward from basic research and use this imaging technique to help patients. This process involves costly steps, so it is necessary to raise funds that go beyond what basic research grants can provide. It was the logical next step to create a spin-off. The name BetaBild was chosen as it represents both the cell type (β) and the imaging technique (‘bild” is Swedish for “image”).
In 2017, thanks to the support of Wallonia Biotech Coaching (WBC) and SOWALFIN, we appointed a manager (Dr Cédric Volanti, former Director at Eurogentec) to help us prepare a competitive business plan and general outline for BetaBild. This plan was recently presented to the Valorisation Committee of the Université Libre de Bruxelles. The next step will be presenting it to the Theodorus Fund, which has already been helping us for several months.
This project has a long history. We hope that in the coming months BetaBild will solidify, and that this will help us make in vivo β cell imaging a reality.”
This article was drafted by guest contributor Amelie Moyaerts from BioWin.