Catherine Verfaillie was very close to being an Olympic athlete in heptathlon, but due to a major knee injury, she had to switch from studying physical education to medicine in her first year of university. It was a blessing in disguise, because Verfaillie is now head of the Stem Cell Institute at KU Leuven (SCIL). In this interview, we take a look at the possibilities of stem cell therapy and we discuss application areas for which stem cell studies are being performed at SCIL. Although we won’t grow new limbs from stem cells within the next 10 years, the possibilities are tremendous.
In a nut shell, The Stem Cell Institute Leuven (SCIL) was founded in 2005, to further develop basic and translational research efforts in stem cell biology. The intermediate and long-term goal are to translate these basic insights in the creation of innovative stem cell-based and -derived therapies for genetic, degenerative, immune-system based, and oncologic disorders, that can be implemented through already well-established clinical programs at the KU Leuven. Since its inceptions SCIL has been progressively adapted in line with the progression in stem cell research.
In addition, a number of translational projects that follow directly from work done in the basic programs are being conducted, including creating disease models, models for drug toxicity assessment; the generation, characterisation and differentiation of iPSC for academic and industrial groups in the GLP KUL-STEM stem cell platform; the acquisition together with the VIB of an automated stem cell and high content screen/high content imaging (HCS/HCI) platform; well as a bone engineering project of Frank Luyten and the heart disease therapy platform by Stefan Janssens and Aernout Luttun, towards phase I and II trials.
First clinical trials
A look at the list of SCIL activities briefly described above and also further on below, shows us that at SCIL stem cells are mainly used as a research platform rather than as a therapy itself. Verfaillie confirms: “Blood stem cells have obviously been used as therapy for a long time, but the use of pluripotent stem cells (PSC)—whether embryonic stem cells or induced pluripotent stem cells (iPSC)—as a therapy is still in a very basic research phase. There are some programs moving to the clinic, though. A clinical trial was published by US teams and one by Japanese teams; they use PSC to treat macular degeneration (the loss of pigment cells in the eye, causing blindness). Also in the US, a clinical trial is scheduled for the treatment of type-1diabetes with b-cells made from PSC. For people with an injury to the spinal cord, a therapy with PSC will probably move to the clinic in the very near future. A phase I clinical trial to treat Parkinson’s disease with PSC might start soon, but it will be conducted very cautiously because of the potential risks of tumor formation.”
It is obviously more complex to make a complete organ than to make one cell type at a time.
Culturing organs, growing limbs and eternal youth
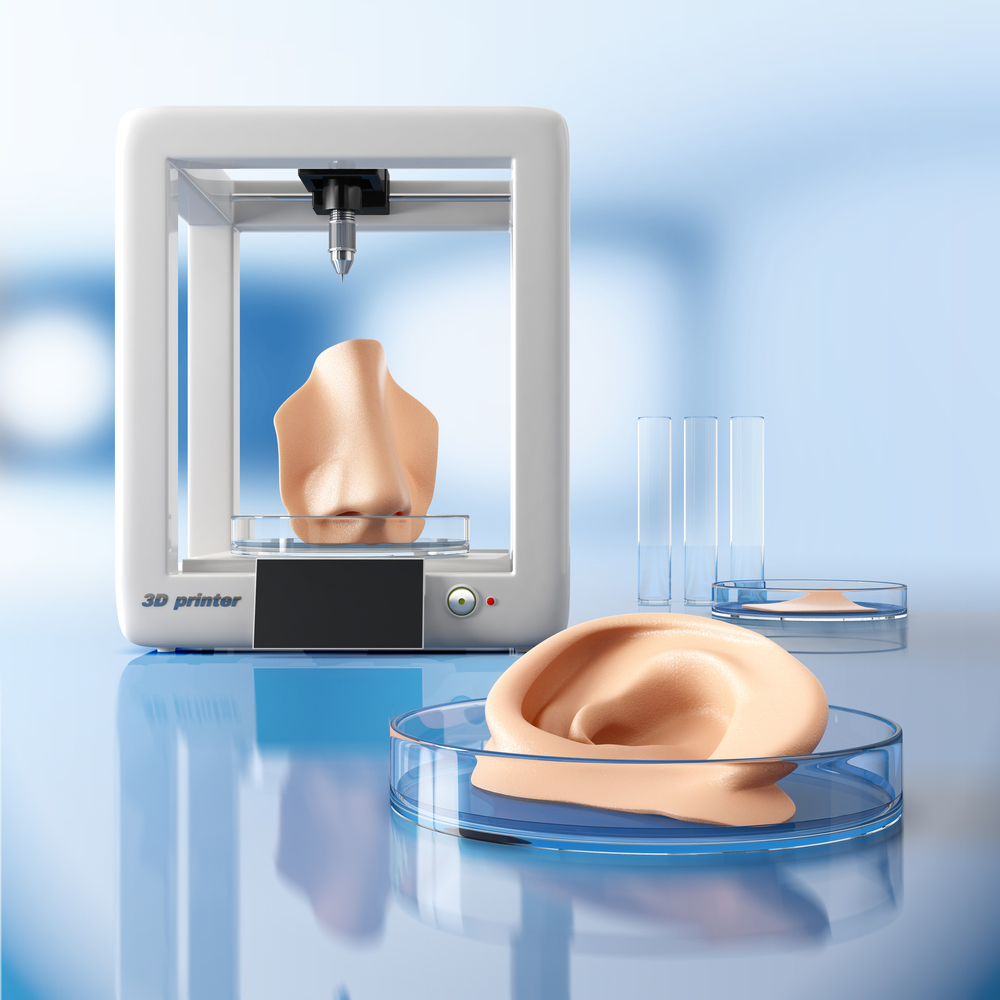
Unfortunately, according to Verfaillie, growing functional organs in the lab, let alone a whole limb, will remain science fiction in the next decades: “It is obviously more complex to make a complete organ than to make one cell type at a time. A liver is an organ of a kilo—that is a tremendous amount of cells—that combines different functions. It is not simple to mimic that. Inducing eternal youth is even more complex, because that would require replacing every single organ of the body. Although science is moving faster and faster and I don’t want to be too negative, I think it will take at least 20 more years before we will be able to grow a kidney in the lab.”
A complex, collaborative approach among people from multiple sites will be necessary to make this work. For example, collaborations with scientists in engineering are set up to create 3D organoids and scaffolds to grow tissue on. Europe, amongst others, is putting a lot of funding into this via the Horizon2020 program.
A brief introduction to the SCIL
The SCIL has a series of programs focusing on very basic and early translational studies, aside from a series of preclinical programs that are looking for application of stem cells clinical or as disease models for drug discovery.
For the basic stem cell biology program, SCIL recruited three group leaders (Kian Koh, Frederic Lluis, Vincent Pasque) into the theme of Pluripotent Stem Cells and Cellular Reprogramming. They study the fundamental mechanisms that regulate stem cell states with a particular focus on pluripotent stem cells (also named embryonic stem cells as they are derived from the inner cell mass of embryos), and the ability of reprogramming adult cells into pluripotent stem cells, a technology that gives rise to the so-called induced pluripotent stem cells or iPS cells) using a range of mammalian systems as well as innovative and state-of-the art technologies in the area of imaging and genomics. A second major area of basic research lays in studies wherein investigators develop progressivly improved methods to guide the stem cells to mature cell types, including cardiac and skeletal muscle, bone, liver and brain. At the same type studies are also being done using ‘adult stem cells’, i.e. stem cells that can be found in most organs, which in contrast have less differentiation and expansion potential compared with pluripotent stem cells. The advantage is however, that they are more easily differentiated into mature cells. These studies include for instance the uterine epithelial stem cells, hematopoietic stem cells or mesoangioblasts.
The hematology program is led by Catherine Verfaillie and Michel Delforge. These teams study how it might be possible to expand hematopoietic stem cells, still the holy grail in this research field. In addition, studies are aimed at understanding how malignant plasma cells in multiple myeloma might escape current therapies with proteasome inhibitor therapy.
The hepatology program is also under the guidance of Verfaillie herself. They spent the last 5 to 10 years trying to make hepatocytes from iPSC. Hepatocytes are the cells very much wanted by biotech and pharmaceutical companies, as well as the cosmetic industry is looking at this because they are not allowed to test their products on animals anymore. The rationale for creating hepatocytes from stem cells is that primary liver-derived hepatocytes cannot be maintained in culture without loss of their mature functions. However, hepatocytes are key for studies on the metabolization and toxicity of drugs. They are also very useful for studying drugs that treat Hepatitis B and C.
Verfaillie’s lab is also involved in the neurodegenerative disease program. They make iPSC from a patient’s cells and develop differentiation protocols to turn the iPSC into cells for studying Alzheimer’s disease, ALS, frontotemporal dementia, Parkinson’s, etc. Potential drugs can be tested on these cells, and disease mechanisms can be revealed. Verfaillie’s team collaborates with a number of other groups including those of Bart De Strooper, Wim Robbrechts, Philip Van Damme, Ludo Van Den Bosch and Wim Van Den Berghe.
The translational cardiomyology program is guided by Maurilio Sampaolesi. Starting from iPSC, he tries to develop both skeletal-muscle cells and heart-muscle cells. The use of such skeletal muscle cells lays in enabling testing of novel drugs for instance for therapy of muscular dystrophy or loss of muscle in ageing, and eventually to repair muscle in muscular dystrophy patients. Creation of cardiac muscle from PSC will allow testing drugs against arrhythmias, and perhaps even muscle patches to repair infarcted hearts.
Maurilio Sampaolesi, Stefan Janssen and Aernout Luttun are developing an innovative cell therapoy approach for cardiovascular disease, by developing a culture platform wherein blood-outgrowth endothelial cells (BOECs) can be expanded and used to revascularize heart tissue in patients with otherwise untreatable cardiac ischemia.
The bone disease program is under the direction of Frank Luyten, one of the founders of Tigenix. His current program is aiming to create bioengineered bone that could be used in for instance non-healing fractures. In addition, such engineered bone could serve as a platform to identify drugs that block or even revert osteoporosis.
The Organoid Culture Platform, under the direction of Hugo Vankelecom, creates organoid cultures from for instance the uterine epithelium, that will enable studying among others uterine cancer and endometriosis. In addition his team has a longstanding research line in stem cells within the pituitary.
Verfaillie concludes: “Really understanding all the communications between stem cells and their environment, and the inherited programs in cells, is still something we have a very limited amount of knowledge about. We have invested quite heavily in trying to solve these basic questions via the basic stem cell biology program. That is really what it takes to move stem cell research to the next level.”