In immunotherapy, the patient’s own immune system is activated to fight cancer cells. Such strategies have been pursued for a few decades and are currently seeing their first commercial applications. However, the quest for new and better ways to help our bodies kill cancer cells is far from over. Dr. Abhishek Garg, a young scientist at KU Leuven, is making a big impact in the field with the development of so-called dendritic cell vaccines for difficult-to-treat tumors such as high-grade glioma (HGG). He presented his work at the Tumor Immunology and Immunotherapy symposium organized by the LKI, Leuven’s Cancer Institute.
No one-size-fits-all solution
The most successful forms of immunotherapy to date involve the use of immune checkpoint inhibitors. Immune checkpoints are used by the body to prevent the immune system from attacking healthy cells. Tumor cells often exploit this mechanism to escape detection. Immune checkpoint inhibitors release the brakes on the immune system, allowing it to attack the cancer cells. Recent research has shown that carcinogen-induced tumors with a high mutational load respond especially well to this type of therapy. For other tumors, such as HGG, checkpoint inhibitors have been found to be less effective. The medical need for treatment of HGG remains high, as currently patients can rely only on traditional chemotherapy.
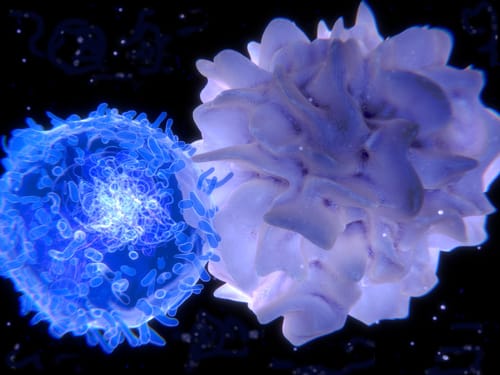
Dendritic cell vaccines offer a promising alternative. Dendritic cells are responsible for processing antigen material and presenting it to the T-cells, which mediate the destruction of the target. When dendritic cells are pretreated in vitro with cancer cell antigens and subsequently injected, the adaptive immune system can be taught to recognize and attack the cancer cells. Previous methods used cancer-specific peptides, or cancer cell lysates obtained by freezing and thawing. However, their success in activating the immune system was limited.
Danger signals lead the way
Dr. Garg’s research into immunogenic cell death (ICD) has created better antigens to prime the dendritic cells. In this method, cultured cancer cells are treated in vitro with hypericin, a compound already used clinically for the fluorescence-based visualization of tumors for resection. The hypericin is activated by light to create oxidative stress, which causes the cells to elicit “danger signals” before they die. The presence of these signals was shown to be essential for successful use in vaccination strategies. Traditionally, such ICD cancer cells are considered to be sufficiently immunogenic by themselves, but adding the intermediary step of using them to treat dendritic cells has drastically increased their immunogenic potential in mouse models.
A one-two punch for HGG
In mice, the vaccine succeeded in slowing down disease progression, but was insufficient to achieve remission. These results were similar to the current standard of care, chemotherapy. However, a chemotherapy treatment followed by an immunization increased the median survival by about 300% and produced a long-term survival rate of about 50%. Presumably, the chemotherapy treatment helps the vaccine overcome the normally strong immunosuppressive effect of tumors. These cured mice stayed healthy even after a new injection of glioma cells, proving the presence of a long-term anti-HGG immune memory.
This strategy offers new hope for HGG patients, who currently have to rely solely on chemotherapy, which eventually fails due to HGG invasion and recurrence. Further research is needed to investigate its effectiveness in humans. To this end, Dr. Garg and his colleagues are developing clinical SOPs for the first trials, which will help this promising therapy take the next step from the bench to the bedside.
Reference
Garg, Abhishek D., et al. “Dendritic cell vaccines based on immunogenic cell death elicit danger signals and T cell–driven rejection of high-grade glioma.” Science translational medicine 8.328 (2016): 328ra27-328ra27.