Antimicrobial resistance (AMR) is one of the greatest threats facing global health today. On the World Health Organization’s 2020 list of ‘Urgent health challenges for the next decade’, AMR is threatening to send modern medicine back decades to the pre-antibiotic era, when even routine surgeries were hazardous.
Fortunately, scientists are hard at work coming up with solutions to this dire problem. In the ongoing series ‘Battling antibiotic resistance’, we’ve previously covered two other options for combatting AMR: a Belgian innovation called Pept-ins™ and the controversial strategy of using bacteriophages.
Recently, bioscience engineers from KU Leuven have developed an antibacterial strategy that works by preventing bacteria from cooperating. The findings are published in Nature Communications.
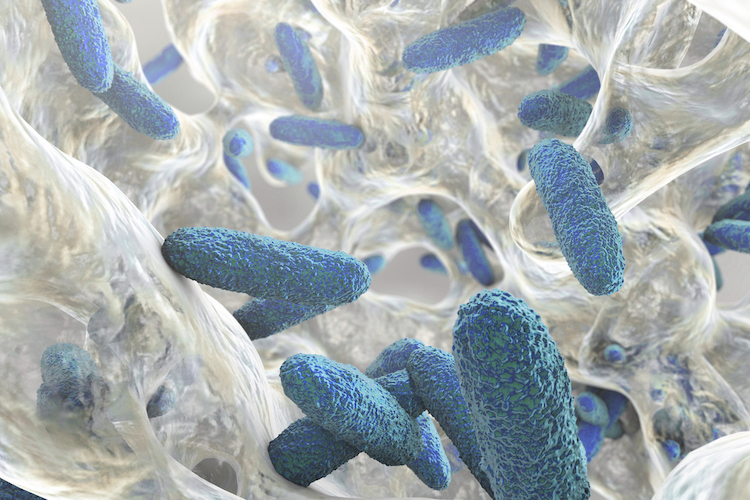
A slimy substance
Traditional antibiotics work by targeting individual bacteria. Problems arise when any one bacterium has a mutation that allows it to survive the onslaught of the antibiotics: with the other bacteria dead, the AMR bacterium is free to multiply and create a whole colony of resistant bugs. With this in mind, the scientists from KU Leuven wondered if there was a way of tackling bacteria at the colony level, rather than individually.
Without their protective slime layer, the bacteria can be washed away by mechanical forces and killed more easily by antibiotics, disinfectants or the immune system. – Hans Steenackers, KU Leuven
Bacteria like to stick together and support each other by forming a protective slime layer, or biofilm, that envelops their entire bacterial community. Biofilms can be nigh on impossible to get rid of and pose major issues in, for example, hospitals and medical implants. Because biofilms protect the colony as a whole, and are problematic in and of themselves, this seemed to be a perfect target for a new antibacterial therapy.
United they stand, divided they fall
Using a chemical, antibacterial substance that had previously been developed at KU Leuven, the researchers were able to demonstrate that blocking slime production in Salmonella bacteria weakens the entire bacterial community. This, in turn, makes it easier to subsequently remove the entire colony without giving rise to any AMR bacteria. Prof. Hans Steenackers, last author of the study, commented:
“Without their protective slime layer, the bacteria can be washed away by mechanical forces and killed more easily by antibiotics, disinfectants or the immune system.”
Steenackers’ team used a so-called evolution experiment to compare anti-slime substance with classic antibiotics.
“We saw that the bacteria, as a group, did not become resistant to our antibacterial substance, while this did happen with antibiotics, and quickly so,” Steenackers explained. “Moreover, we showed those bacteria that were resistant to the new antibacterial substance became outnumbered by non-resistant ones.”
The reason the bacteria don’t develop resistance to the anti-slime substance is simple: producing slime costs energy. This means that any bacteria that become resistant to the anti-slime substance are able to produce a protective biofilm for themselves and their non-resistant neighbors, but in doing so they quickly become outcompeted by the neighbors they are protecting, free of charge. They are simply overrun by surrounding non-resistant bacteria that spend their energy on growth and multiplication rather than costly slime production.
In the long term, this concept can also be used to develop alternatives to antibiotics. – Hans Steenackers, KU Leuven
“In contrast to traditional antibiotics, this substance therefore does not cause selection for, but against, resistance,” Steenackers summarized. “Antimicrobial treatments that stop bacteria from working together can therefore be a viable solution to the current problem of antibiotic resistance.”
How to apply this new substance?
With the evolutionary study concluded, the next step for the researchers will be to determine how best to use this anti-slime substance to combat AMR. Steenackers stated:
“Our aim is to introduce these new antimicrobials into clinical practice. They can be used as a preventive medicine in the form of a pill, or as a coating on implants to reduce the risk of infections.”
The substance could of course also be used in a complimentary fashion together with more traditional antibiotics. The researchers also foresee potential for the anti-slime substance in agricultural, industrial or even household applications. To realize the potential of their discovery, the team will be collaborating with experts in these different fields. They have also already begun further studies to evaluate whether the substance can be used in other bacterial species and for other types of bacterial collaboration.
“In the long term, this concept can also be used to develop alternatives to antibiotics.” Steenackers concluded.
Quotes courtesy of KU Leuven.