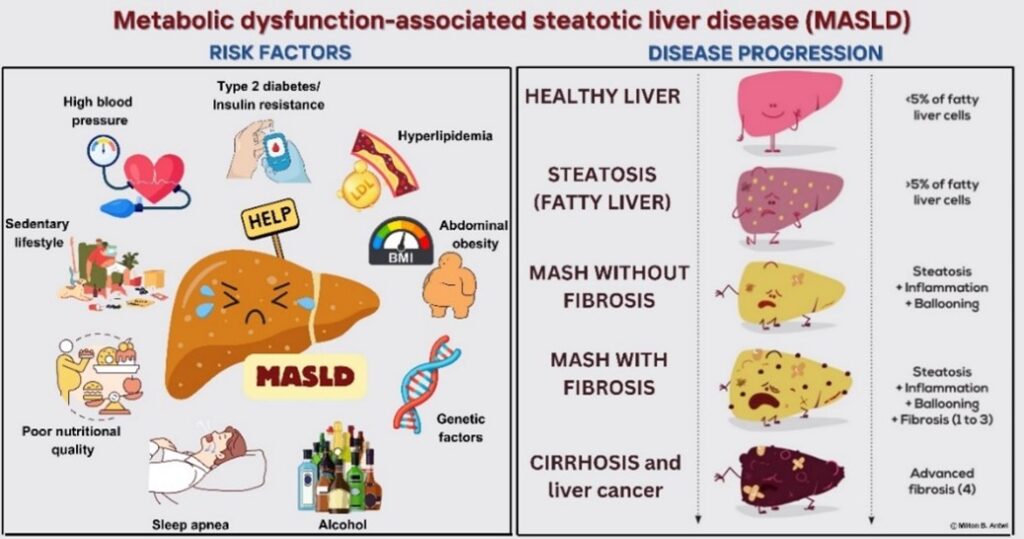
MASLD-associated risk factors and disease progression to liver cancer
Patients with MASLD are a diverse group, often battling obesity, type II diabetes, and dyslipidemia (high cholesterol or fat). Without intervention, MASLD can eventually progress into liver cancer, a devastating diagnosis that claims over 800,000 lives globally each year. MASLD typically lacks obvious symptoms early on and so goes unnoticed. More visible symptoms like jaundice (yellowing of the skin and eyes) and abdominal swelling become apparent only in advanced stages. This makes early detection of the disease vital. Therefore, doctors recommend testing individuals who are overweight and present with elevated liver enzyme levels in their blood tests. To diagnose MASLD, physicians rely on a trio of key tests: blood tests that check for high liver enzymes, imaging tests such as ultrasound or magnetic resonance imaging (MRI) that scrutinize the liver’s appearance, and more recent innovations like fibroscan and transient elastography that measure liver fat content.
Why does MASLD affect men and women differently?
Recent studies have delved into why MASLD affects genders differently, focusing particularly on disease development. Initially, men are more susceptible to developing a fatty liver compared to women. However, this changes post-menopause, when women’s risk not only catches up but may exceed that of men. The explanation lies in the role of female sex hormones, particularly estrogen, which protect the liver by guarding against fat buildup. When estrogen levels drop during menopause, this protective barrier weakens, making the liver more prone to fat accumulation. This insight has spurred interest in estrogen supplements as a potential preventive treatment for post-menopausal women, a strategy showing promise in lowering the risk of developing MASLD. On the other hand, for women in their mid-thirties with higher levels of testosterone, the risk of progression to severe stages of liver inflammation and cirrhosis doubles. The reasons behind the impact of high testosterone in these cases remain a puzzle that researchers are eager to solve.
Men face their own challenges with hormonal changes as they age. Declining testosterone levels, a typical part of aging, are linked to a heightened risk of developing fatty liver disease. This connection is partly due to the relationship between low testosterone and obesity. Men diagnosed with MASLD typically have lower testosterone levels than those without the condition, and these reduced levels are independently linked to a higher risk of MASLD. While testosterone replacement therapy is gaining attention for its benefits on insulin resistance and obesity, its direct impact on MASLD warrants further investigation.
Given the crucial role hormones play in MASLD, especially for those undergoing gender-affirming treatments, medical approaches need to be carefully considered. This is particularly important for individuals with existing liver conditions to prevent exacerbating their health issues.
Current treatments for MASLD
Current evidence suggests that a weight loss of at least 5% can significantly improve liver health in cases of MASLD, with a 7-10% weight loss potentially impacting MASH (liver inflammation) and fibrosis. Achieving this requires increased physical activity and a better diet. While structured lifestyle interventions have proven effective, they yield modest results: only 5-10% of patients achieve their target weight loss within the first year, and less than half maintain this weight loss five years later.
For obese patients, weight-loss surgery, presents a possible solution to improve MASLD. Those with physical disabilities or other medical conditions might need medications specifically tailored to address MASLD or MASH. Several promising medications are in phase 3 clinical trials, though awaiting results and FDA approval. On March 14, 2024, the FDA approved Rezdiffra (also known as Resmetirom) as the first MASH targeted drug for use in the United States. Other current treatments for MASLD patients include medications that can manage their blood glucose, blood pressure, and lipids levels.
Gender personalized medicine: the way forward
The prevalence of sex hormone abnormalities in MASLD patients underlines the significant role these hormones play in managing not just the liver but also the metabolism of lipids, carbohydrates, and proteins. In men, low testosterone levels have been identified as a risk factor for both MASLD and MASH. Therefore, monitoring testosterone levels throughout treatment is recommended. However, the effects of testosterone on factors like blood pressure and sleep apnea mean that testosterone replacement may not be suitable on its own. Instead, evidence suggests that using GLP-1 agonists like semaglutide, which can improve testosterone levels through weight loss, might be a viable strategy.
Currently, no gender-specific pharmacotherapy is approved for women with MASLD and MASH. Ongoing clinical trials are testing inhibitors that target pathways that cause fat accumulation (namely acetyl-CoA carboxylase, diacylglycerol O-acyltransferase, and stearoyl-coenzyme A desaturase 1). These pathways are of particular interest for treating MASLD in postmenopausal women due to the specific increase in fat or lipid synthesis triggered by estrogen deficiency.
Understanding MASLD through a gender-specific lens offers a clearer, more nuanced view of its complexities, emphasizing the need for tailored treatment strategies. Future clinical trials should compare the effectiveness of therapeutic agents between males and females. As research progresses, the hope is that these insights will lead to breakthroughs in treatment options, providing new hope for those battling this silent epidemic.
References
- Younossi ZM, Golabi P, Paik JM, Henry A, Van Dongen C, Henry L. The global epidemiology of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH): a systematic review. Hepatology. 2023;77(4).
- EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;
- Hutchison AL, Tavaglione F, Romeo S, Charlton M. Endocrine aspects of metabolic dysfunction-associated steatotic liver disease (MASLD): Beyond insulin resistance. J Hepatol. 2023 Dec;79(6):1524-1541
- Lonardo A, Nascimbeni F, Ballestri S, Fairweather DL, Win S, Than TA, et al. Sex Differences in Nonalcoholic Fatty Liver Disease: State of the Art and Identification of Research Gaps. Vol. 70, Hepatology. 2019.


