Fast Healthcare Interoperability Resources (FHIR) is a widely adopted framework for efficient and secure sharing of health-related data. It consists of a set of rules that enable efficient and secure sharing of health-related data between different systems and applications. It is complementary to another commonly used healthcare data standard OMOP CDM, which has different functionalities.
Read this article to find out more about the differences and compatibilities between FHIR and OMOP CDM!
FHIR attempts to represent healthcare systems using a fixed set of resources, each representing a specific, relevant aspect of a healthcare system. Resources can represent: actors (such as the patient, practitioner, and hospital organization); actions (such as observation and procedure); and data extracted from these aspects (such as clinical reporting to payer resources, lab requests, and admission information). All resources have well-defined structures and can be linked to each other through references, generating an interconnected system.
To illustrate the concept of resources and references, let’s consider a simplified example: a patient with a COVID-19 infection entering a hospital to get treatment. The patient is a ‘resource’, potentially suffering from several conditions (for example obesity or diabetes), which are also ‘resources’. The hospital and the practitioner carrying out the treatment are both resources as well, as is the procedure performed to treat the patient. All resources can be linked through references, which indicate how the resources are connected. For instance, the patient is subject to a procedure and the practitioner is performer of this procedure.
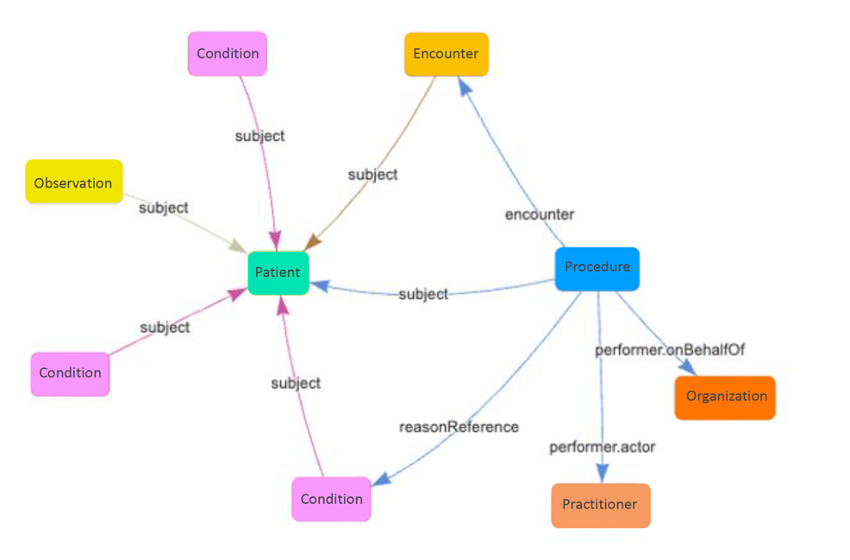 Credit: Tiro health
Credit: Tiro health
Of course, solving interoperability with a fixed set of resources doesn’t entirely satisfy the complex needs of the healthcare IT industry. This is why FHIR adopts an 80/20 principle with a base layer of fixed resources that define 80% of the information that needs to be exchanged and 20% of well-documented procedures to make extensions to these models, enabling customization to various healthcare use cases.
When customization is needed
The flexibility of the FHIR resources is both a strength and a challenge. The wide range of resources provided by FHIR can make it too broad or generic for specific use cases. To address this, FHIR profiles and implementation guides come into play allowing for customization, tailoring the standard to specific requirements and contexts. They define additional constraints, extensions, and rules that refine the use of resources, making them more relevant and specific. By standardizing the data layer in your IT system with FHIR, your infrastructure transforms into a valuable commodity. This fosters a dynamic ecosystem where all players can collaborate and progress can be achieved faster.
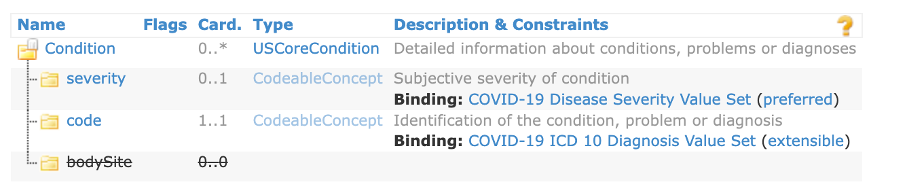
Let’s come back to our COVID-19 example. In case no universal code was available, the condition might be described slightly different in various healthcare settings, complicating collaboration and large-scale analysis. To solve this issue, a FHIR profile is available (the US profile for COVID-19), with a fixed code representing the condition resource (ICD-10 code: U07.1). The severity must be coded as well, using a predefined set of SNOMED codes. The profile ensures that each COVID-19 condition is captured in the same way irrespective of the institution, improving data consistency and meaningful large-scale analysis.
Credit: Tiro health
Capturing data with questionnaires
The above examples show how FHIR provides structured data representation. However, there is still the need for a solution that facilitates capturing the standardized data across different healthcare settings. This is where FHIR questionnaires come into play. They can be designed and used by clinicians, knowledge institutions etc. to formulate essential information to be gathered from patients for specific purposes while software developers can use these specifications to build tools, such as healthcare applications to track COVID-19 infections.
Exchanging data for better health
FHIR enables interoperability by providing standardized methods for querying, retrieving, updating, and deleting healthcare data. By following modern web standards, FHIR becomes accessible and compatible with a wide range of platforms and technologies, allowing for effective collaboration, interoperability, and data-driven decision making across the healthcare ecosystem.

Credit: Tiro health
This fosters a dynamic ecosystem where all players can collaborate and progress can be achieved faster, with everyone operating according to the same standards and agreements.
Interested in learning more about the use of FHIR data models in a clinical context? Find out more about the topic here.