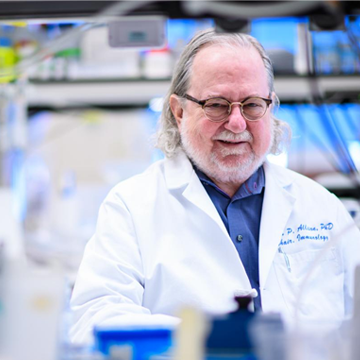
Dr. James Allison has dedicated his career to improving our fundamental understanding of how the adaptive immune system works. Much of what you will find on T cells in today’s immunology textbooks is the result of his work. Dr. Allison’s focus on basic research has also impacted the lives of cancer patients tremendously. By unraveling the mechanisms that drive the immune system, he has pioneered new and effective strategies to fight solid tumor growth. He was selected by a group of scientific peers to receive the 2018 Dr. Paul Janssen Award for Biomedical Research, the prize established by Johnson & Johnson in 2004 to honor the memory of Dr. Janssen. The prize has so far recognized 15 outstanding scientists, of which two have gone on to win the Nobel Prize. On September 6th, Dr. Allison presented his work at Janssen’s Beerse campus.
By Amy LeBlanc
The immune system not only protects the body against pathogens like bacteria or viruses, but also has the potential to destroy cancer cells. In theory, T cells would be perfectly suited to fight cancer as they patrol the body looking for intruders to destroy: they keep track of past threats they have encountered so they are equipped to fight them in the future. However, tumor cells have the ability to disguise themselves and escape T cells.
Allison’s work has been paramount in understanding how T cells function. One of his first major discoveries was the ignition switch for the adaptive immune system, a combination of two molecules called the T cell receptor and CD28. Importantly, he later discovered that these cells have a brake, or ‘checkpoint’: the molecule CTLA-4. This system prevents healthy cells from becoming a target but is abused by cancer cells trying to survive.
To find out more about cancer immunotherapy, read our White Paper!
Releasing the brakes
Allison and his team quickly realized that their discovery could provide the foundation for a brand-new type of immunotherapy; new ‘immune-system’ drugs could release these T cell brakes and would be applicable to treat any type of cancer. This was far from a new concept, as early attempts to treat cancer with immuno-stimulation date back to the 19th century, but it was the first time the theory could be made into a reality.
A trial on 5.000 patients revealed that they who were alive after 3 years, still remain disease-free today. – James Allison
With ipilimumab, Allison created the first human antigen against CTLA-4, successfully releasing the brakes. This first immunotherapy treatment changed the field of cancer research fundamentally. For decades, advances in cancer treatment had consisted of prolonging the expected survival, by weeks or months. In ipilimumab’s clinical trials, all traces of cancer disappeared in 20% of the metastatic melanoma patients who received this new type of therapy. “A trial on 5.000 patients revealed that they who were alive after 3 years, still remain disease-free today,” Allison states.
Building on these initial discoveries, other research groups discovered a second checkpoint with a very different mechanism of action, called PD1. In subsequent years, countless clinical trials investigated combinations of drugs targeting both checkpoints. Some of these trials have improved upon the expected outcomes for melanoma patients, with early results showing an increase of the percentage of long-term disease-free patients to 50%.
Beyond the checkpoints
Dr. Allison’s goal is now to do better, both for the significant number of patients who don’t respond to the checkpoint inhibitors, as well as for the patients with difficult to treat cancers such as glioblastoma or pancreatic cancer. “We know the basic lessons, now we should identify what their tumor landscapes are and put the puzzle together,” he explains.
According to Allison, the way forward is leveraging new technologies to understand everything at a more granular level. To achieve this, he founded the Immunotherapy Platform at the MD Anderson Cancer Center, the most highly-regarded cancer institute in the USA. Together with Dr. Sharma, his partner both professionally and personally, he collects and investigates tissue biopsies of both responders and non-responders to the checkpoint inhibitors.
Through characterization, the T cell populations in these tissue samples have allowed associations to be determined between cell types and treatment outcomes. The results of these studies have led, among other breakthroughs, to the discovery of the Inducible T cell costimulator (ICOS) protein. This molecule, expressed on activated T cells, can be used as a pharmacodynamic marker for ipilimumab activity and potentially even as a target to improve the efficacy of anti-CTLA-4 therapies.
We know the basic lessons, now we should identify what their tumor landscapes are and put the puzzle together. – James Allison
It is clear, when listening to Dr. Allison, that his fighting spirit and scientific curiosity are far from spent; his presentations at both the Belgian and US award ceremonies were an inspiration to all who attended. He continues to chip away at the secrets of the immune system. By now, advances in the immunology field are coming in at such a pace that text-books can’t keep up with the rate of scientific publications. In this wave of innovation, Dr. Allison’s work stands as a shining example of how the fundamental investigation of biological processes can lead to the development of transformative therapies.